Under-fueling and Relative Energy Deficiency in Sport: Why Your hemaglobin A1c Might Be High, Even If You’re an Endurance Athlete
The Paradox of the “Healthy” Endurance Athlete
Endurance athletes are often viewed as models of health and performance. Preparing for an ultramarathon, century ride, or Ironman requires far more than dedication and countless hours of training. It demands planning, recovery, nutrition, and careful structure. From the outside, it looks like the embodiment of discipline and resilience.
Yet in nearly a decade of working as a Registered Dietitian at the intersection of eating disorders and endurance sport, I’ve seen a different reality play out in the lab results of athletes. Many arrive in my office confused by findings such as elevated LDL cholesterol or rising hemoglobin A1c, which are markers more commonly associated with metabolic disease.
The typical medical response given to them by their doctors is to “eat healthier and exercise more.” However, in this population, that recommendation is not only incorrect but downright harmful. Advice like this can lead to further restriction, orthorexia, and even deeper energy deficiency. Changes in lab values like cholesterol or A1c aren’t signs of laziness or poor dietary choices — they’re signals of a body under energetic strain. I wrote more about this paradox in my article on underfueling and cholesterol, and how it can silently shift an athlete’s metabolism.
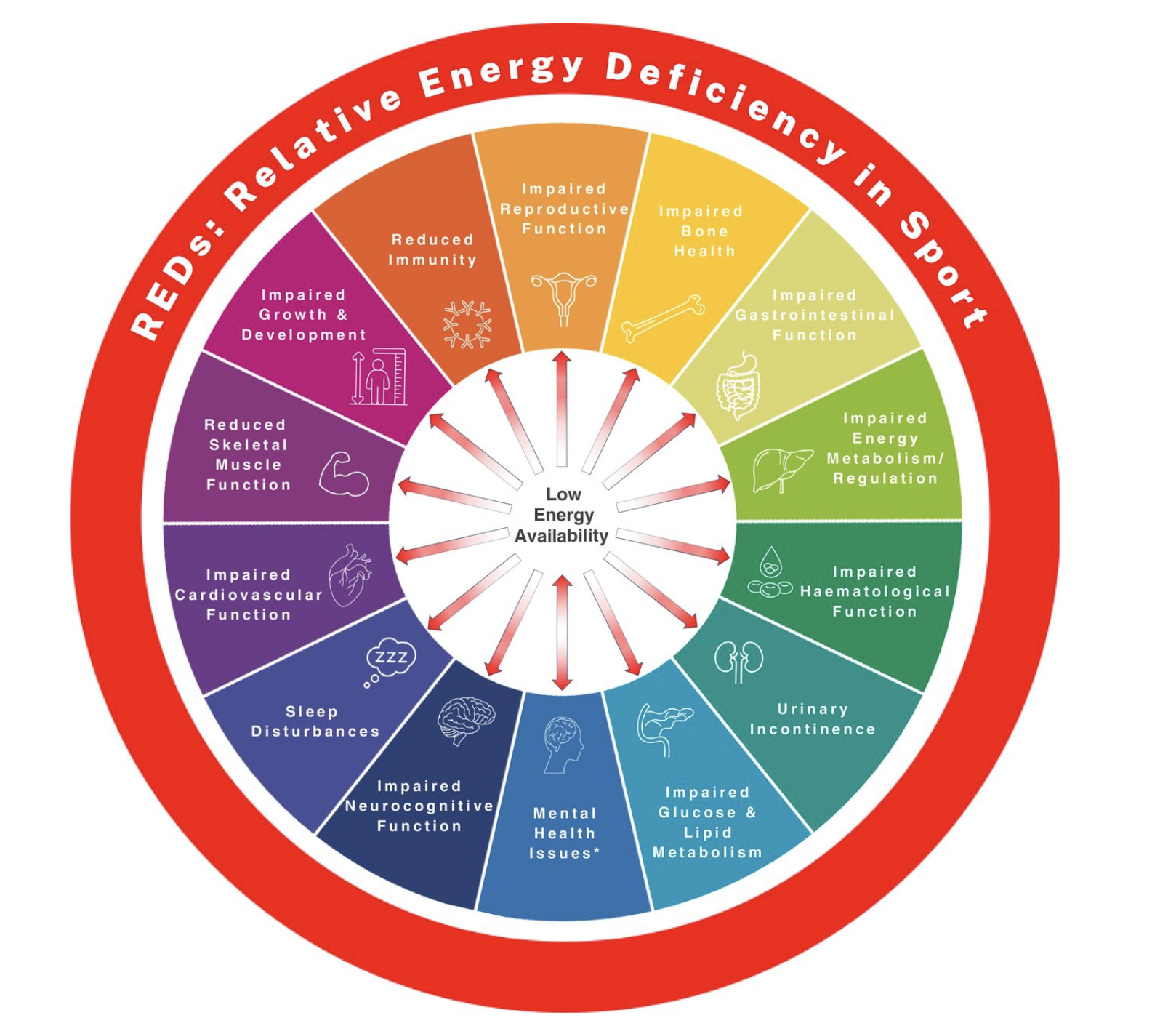
This pattern is often explained by Relative Energy Deficiency in Sport (REDs), a state of chronic low energy availability and physiological stress. REDs doesn’t simply suppress performance and blunt recovery; it alters physiology at a fundamental level, shifting hormones, lipid metabolism, and glucose regulation, and can have lifelong health consequences.
What Is REDs?
REDs Health Conceptual Model. The effects of LEA exist on a continuum. While some exposure to LEA is mild and transient termed adaptable LEA (arrow depicted in white), problematic LEA is associated with a variety of adverse REDs outcomes (arrow depicted in red). *Mental Health Issues can either precede REDs or be the result of REDs. LEA, low energy availability; REDs, Relative Energy Deficiency in Sport.
In the early 1990s, researchers observed that female athletes with eating disorders often developed amenorrhea (missed menstrual cycles) and osteoporosis. This became known as the Female Athlete Triad. Over the last 25 years, research has shown that under-fueling combined with high training loads doesn’t just affect female athletes or bone health—it impacts athletes of all genders and affects nearly every system in the body.
In 2014, the International Olympic Committee (IOC) released a consensus statement expanding the Triad into Relative Energy Deficiency in Sport (REDs).¹ At its core, REDs stems from low energy availability—consistently burning more calories than you consume. It doesn’t just impact an athlete’s ability to recover; it can end careers and alter long-term health outcomes.
REDs affects multiple systems: metabolic, hormonal, immune, cardiovascular, and musculoskeletal. Recent research has also highlighted the role of systemic stress and the impact of low carbohydrate intake as a key driver of REDs—not just overall low energy availability.²
You might think, “I’m not an Olympian or a professional athlete—this doesn’t affect me.” Unfortunately, research tells a different story:
A 2024 meta-analysis found that 44.7% of all athletes show signs of low energy availability (LEA).³
47.6% of endurance trail runners report consuming fewer carbohydrates than recommended for endurance performance.⁴
73% of male and female collegiate distance runners fail to meet daily carbohydrate recommendations.⁵
Even short-term LEA (lasting days to weeks) can disrupt thyroid function, slow metabolic rate, and decrease protein turnover and muscle recovery.⁶
Only 54.7% of non-elite endurance athletes meet carbohydrate recommendations.⁷
As you can see, REDs is far more common and easily overlooked than most people realize. The body is highly adaptive; its primary goal is survival. When energy and nutrients are limited, it reallocates resources to keep vital systems functioning. Hormones shift, recovery slows, and metabolic pathways adjust in ways that can quietly compromise long-term health. While many athletes first notice REDs through fatigue, mood changes, or recurrent injuries, bloodwork often reveals the warning signs earlier.
Issue #1: Cholesterol Drift
In a previous article, I highlighted how training in an underfed state can paradoxically raise LDL cholesterol. When the body is in an energy deficit, the liver ramps up production of circulating lipids as an alternative energy source. The result: endurance athletes who appear to be doing everything right—fueling with “healthy” foods and training consistently—can still develop cholesterol patterns that resemble those seen in individuals at higher risk for heart disease.
These changes reflect that their body is under genuine physiological stress. While the root cause is different from traditional cardiovascular disease, they remain a meaningful health concern. One that won’t be solved by simply exercising more or “eating better”
Issue #2: HbA1c and the Carbohydrate Gap
Another marker I see in my athletes with REDs is an elevated hemoglobin A1c (HbA1c). This is best known as a blood marker for diabetes risk. It measures how much sugar has been stuck to your red blood cells over the past ~3 months. In inactive people, a high HbA1c usually points to insulin resistance and a higher risk for developing Type 2 Diabetes. But for endurance athletes, especially those who aren’t eating enough carbohydrates, the story is very different.
Before we dive in, let’s define a few key terms:
Glucose is the body’s primary fuel source. When you eat carbohydrates, whether this is from fruit, starchy vegetables, grains, beans, or candy, it will all eventually be turned into glucose.
Glycogen is stored glucose and water. Muscles and the liver both contain glycogen, but for different jobs. Muscles use it locally to fuel contractions and movement. Liver glycogen is more like a “backup generator” that keeps blood sugar stable for the brain and other organs.
Insulin is the hormone that moves glucose out of the bloodstream and into tissues. If the body becomes less responsive, that’s called insulin resistance.
Fasted or low-carb training pushes the body to burn more fat, and causes muscles to become temporarily insulin resistant, aka worse at pulling glucose from the blood, resulting in higher blood glucose.
Energy Use During Exercise
During training, the body uses a mixture of glucose, muscle glycogen, fat, amino acids, and phosphocreatine. Which system dominates depends on intensity, oxygen availability, and duration. 7
Low–moderate intensity (Zone 1-2): primarily fat and blood glucose
Higher intensity (Zone 3-4): muscle glycogen and blood glucose
High intensity and short bursts (Zone 5): muscle glycogen and phosphocreatine
Long duration (2+ hours): increasing reliance on fat, but glycogen remains crucial for sprints, climbs, and surges.
When there isn’t enough glycogen or glucose available, the body begins to break down protein and amino acids from muscle to create glucose. This process impairs training adaptation and increases injury risk.
Why HbA1c can rise in athletes who under-fuel:
Stress hormones (cortisol, adrenaline): Intense exercise and low energy availability raise stress hormones, which tell the liver to dump more glucose into the bloodstream, while making tissues less responsive to insulin. Thus raising A1c levels.
Post-exercise insulin resistance: As we learned above, if there isn’t enough glycogen, the body will release fat into the bloodstream for fuel. This temporarily makes your muscles less responsive to insulin, meaning your muscles don’t absorb sugar as efficiently for a short time after training. When you don’t eat enough carbs before, during, or after training, this can prolong this “temporary” insulin-resistant state for 1-2 days. For athletes training daily, that can mean chronic, low-grade insulin resistance. Combine insulin resistance with stress that results in higher blood glucose, and we have the perfect storm to cause A1c to creep up over time. (8)
Fuel inflexibility: When glycogen is low, muscles may have a harder time switching between fat and carbs. Over time, this makes them less efficient at clearing glucose from the blood after meals, leading to higher HbA1c.
Red blood cell turnover: Your A1c doesn’t just reflect blood sugar; it’s also influenced by how long your red blood cells (RBCs) live. Normally, red blood cells circulate for about 3-4 months before being replaced. If you can’t make RBCs as quickly enough because of under-fueling, low iron, or hormonal changes from REDs—older cells linger longer, giving glucose more time to attach. That can make HbA1c appear higher, even if blood sugar itself isn’t elevated.
The paradox:
An endurance athlete who restricts carbohydrates—intentionally or not—may show an “elevated” HbA1c despite being highly insulin sensitive. It doesn’t mean diabetes; it means the body is under strain and needs more fuel.
The Broader Picture of REDs
REDs affects far more than lab work. It’s not just about fatigue or performance dips — it’s a whole-body energy crisis that impacts nearly every physiological system. Its consequences span physical, hormonal, and psychological health.
Skeletal System (Bone Health)- increased risk of stress fractures, delayed wound healing, and early-onset osteoporosis
Reproductive hormones- reduced libido, low testosterone, menstrual dysfunction, and infertility.
Metabolic and endocrine- decreased metabolic rate, cold intolerance, abnormal thyroid function, and loss of appetite
Cardiovascular health- low resting heart rate, dizziness, low blood pressure, low heart rate variability (HRV), and altered lipid metabolism
Immune function- frequent colds or infections, long recovery from illness or injury, and increased systemic inflammation
Gastrointestinal (GI) health- bloating, constipation, or diarrhea, low appetite, slowed digestion, GI distress when training
Urinary and pelvic health- urinary incontinence, pelvic floor weakness
Neuromuscular function- muscle loss, reduced strength, poor coordination, overuse injuries, increased soreness, and fatigue
Psychological and cognitive- increased anxiety and depression levels, decreased motivation, impaired concentration, sleep disturbances
Performance- plateauing in training, reduced power, poor endurance adaptation, and levels of higher perceived exertion during training
As you can see, REDs is a cascade of adaptations designed to keep you alive—but not necessarily thriving. The longer it persists, the more systems become compromised. Blood markers like cholesterol and HbA1c may serve as early warning signs of physiological stress—signals of something potentially serious that shouldn’t be ignored.
Where We Go From Here: Practical Takeaways for Athletes
Fuel to match your training load—especially with enough carbohydrates before, during, and after training. Adjust nutrition as training volume increases.
Use labs as feedback, not judgment. A “borderline” HbA1c or cholesterol value might be your body’s way of saying, I need more fuel.
Look for patterns, not single numbers. Combine bloodwork with performance metrics, recovery, mood, and injury patterns.
Seek professional support. Surround yourself with a team of providers familiar with REDs—ideally a Registered Dietitian, physical therapist, medical doctor, and coach. Don’t let under-fueling steal the joy from training, your sport, or your career.
Final words…
After nearly a decade of working with athletes, nothing is harder than watching under-fueling steal the joy from training and sport. It’s even harder knowing that something so preventable can jeopardize long-term health—or even cut a career short.
Athletes thrive on pushing boundaries and seeing what they’re capable of. But sometimes, the hidden cost of that discipline is chronic under-fueling. REDs isn’t just about low energy—it’s about the ripple effects across every system in the body, from bones and hormones to cholesterol and HbA1c.
At EVOLVE, our philosophy is that performance and health don’t have to be a trade-off. With the right fueling and recovery strategies, athletes can protect their health, perform at their best, and keep doing what they love for years to come.
Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, Meyer N, Sherman R, Steffen K, Budgett R, Ljungqvist A. The IOC consensus statement: beyond the Female Athlete Triad--Relative Energy Deficiency in Sport (RED-S). Br J Sports Med. 2014 Apr;48(7):491-7. doi: 10.1136/bjsports-2014-093502. PMID: 24620037.
Jeukendrup AE, Areta JL, Van Genechten L, Langan-Evans C, Pedlar CR, Rodas G, Sale C, Walsh NP. Does Relative Energy Deficiency in Sport (REDs) Syndrome Exist? Sports Med. 2024 Nov;54(11):2793-2816. doi: 10.1007/s40279-024-02108-y. Epub 2024 Sep 17. PMID: 39287777; PMCID: PMC11561064.
Gallant TL, Ong LF, Wong L, Sparks M, Wilson E, Puglisi JL, Gerriets VA. Low Energy Availability and Relative Energy Deficiency in Sport: A Systematic Review and Meta-analysis. Sports Med. 2025 Feb;55(2):325-339. doi: 10.1007/s40279-024-02130-0. Epub 2024 Nov 1. PMID: 39485653.
Henninger K, Pritchett K, Brooke NK, Dambacher L. Low Energy Availability, Disordered Eating, Exercise Dependence, and Fueling Strategies in Trail Runners. Int J Exerc Sci. 2024 Jan 1;16(2):1471-1486. doi: 10.70252/FFDK5934. PMID: 38288400; PMCID: PMC10824294.
Beermann, B. L., Lee, D. G., Almstedt, H. C., & McCormack, W. P. (2020). Nutritional Intake and Energy Availability of Collegiate Distance Runners. Journal of the American College of Nutrition, 39(8), 747–755. https://doi.org/10.1080/07315724.2020.1735570
Jeppesen JS, Hellsten Y, Melin AK, Hansen M. Short-Term Severe Low Energy Availability in Athletes: Molecular Mechanisms, Endocrine Responses, and Performance Outcomes-A Narrative Review. Scand J Med Sci Sports. 2025 Jun;35(6):e70089. doi: 10.1111/sms.70089. PMID: 40539747; PMCID: PMC12180388.
Masson G, Lamarche B. Many non-elite multisport endurance athletes do not meet sports nutrition recommendations for carbohydrates. Appl Physiol Nutr Metab. 2016 Jul;41(7):728-34. doi: 10.1139/apnm-2015-0599. Epub 2016 Mar 1. PMID: 27176786.
Flockhart M, Larsen FJ. Continuous Glucose Monitoring in Endurance Athletes: Interpretation and Relevance of Measurements for Improving Performance and Health. Sports Med. 2024 Feb;54(2):247-255. doi: 10.1007/s40279-023-01910-4. Epub 2023 Sep 2. PMID: 37658967; PMCID: PMC10933193.